ASPIRIN
Here is a brief explanation on how aspirin works. Aspirin inhibits a substance called cyclooxygenase and the prostaglandins that follow it in a chemical cascade. Cyclooxygenase is an enzyme that helps break down arachidonic acid to prostaglandins. Aspirin stops this enzyme from doing its job. The cells in your body respond to various stimuli in order to bring about a reaction that will help rectify or signal what is going on. Cells respond to activating stimuli by remodeling their cellular membranes to generate biologically active lipid mediators that serve as short range signaling agents. Each prostaglandin and thromboxane that is produced serves a purpose. For example, PGI2 causes vasodilation and inhibits platelet aggregation. TXA2 causes vasoconstriction and promotes platelet aggregation,which is the belief doctors have about it use and heart attack prevention. They feel if you inhibit this from being formed that it will keep the blood thinner and keep it from clotting.
As one can see there are many other things inhibited that are beneficial. PGD2, PGE2, and PGF2 are involved in vasodilation and causing of edema. PGE2 and PGI2 are involved in the production of mucus in the stomach, which protects it from ulceration. The other side of the equation shows leukotrienes. LTC4, LTD4, and LTE4 are involved in vasoconstriction, bronchospasm and increased vascular permeability. They also increase secretion of bronchial mucus and produce wheal and flare reactions in skin. One of the potential negative effects of aspirin and its inhibition of cyclooxygenase is that it can redirect the breakdown of arachidonic acid throught the other side of the equation which will lead to higher production of the leukotrienes and the action that they potentiate.
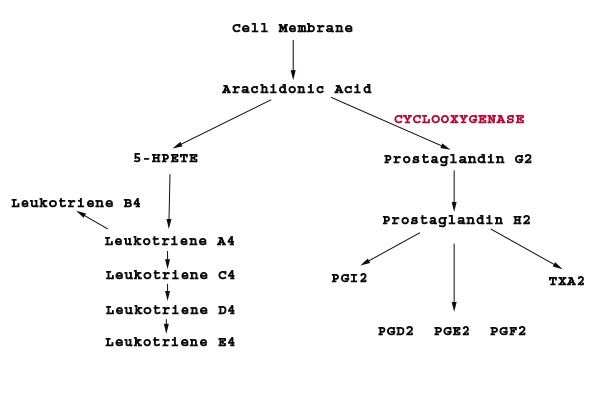
The picture above shows the enzyme cyclooxygenase (in red). This is what aspirin inhibits. Inhibition of this enzyme will block the formation of all of the prostaglandins that follow in this cascade. The blockage of cyclooxygenase is irreversible. This is important when discussing platelets. Platelets are cells that lack nuclei, therefore cannot synthesize new cyclooxygenase enzyme. This enzyme blockage will persist for the lifetime of the platelet cell (3 to 7 days). If the body needs to clot, it has to manufacture new platelets. Blocking the ability of platelets to clot can be a very dangerous situation.
Given this information, you can now arm yourself to better question your doctor. Below I have included some interesting information pertaining to aspirin and its use in heart attacks. Educate yourself to help decide if this is the proper treatment or advice for you. I am confident that after learning all you can about the issue you will not chose this road that so many have been blindly lead down.
At the end of the articles there is a list of Natural Alternative to Aspirin.
The most common adverse effect from therapeutic anti-inflammatory doses of aspirin is gastric upset. Chronic use results in gastric ulceration, upper gastrointestinal bleeding (a loss of as much as a teaspoon of blood per day), and renal effects, including acute renal failure and interstitial nephritis. Aspirin increases bleeding time also. Some people may experience asthma because of the cascade redirection. Depending on how much aspirin you take you may experience tinnitus (ringing in the ears), vertigo, hyperventilation, and respiratory alkalosis. It has also been known to cause metabolic acidosis, dehydration, hyperthermia, collapse, coma and death. Children with viral infections are at risk of develping Reye's syndrome (hepatic fatty degeneration and encephalopathy) if given aspirin.
WARNING ! THE ONLY THING THAT PREVENTS THE STOMACH FROM DIGESTING ITSELF IS THE MUCOUS LINING! Are you trying to kill yourself through the chronic use of ASPIRIN??? The Center for Disease Control in Atlanta has documented for over a decade that 17,000 to 20,000 deaths a year are a direct result of a hemmoraging of the stomach as a result of aspirin, IN ANY FORM! Aspirin dissolves the mucous lining of the stomach, and when in the blood stream prevents and blocks the replacment of that mucous!
Doctors are pushing aspirin because it thins the blood, keeping it flowing smoothly so dangerous clots don't form. They key on it for its ability to prevent platelets from sticking together and causing clots, which they feel will help prevent heart attacks. This is a typical "treating the symptom and not the cause" mode of thinking that plagues the medical field.
There are safer and better ways to accomplish this. Anyone that understands the physiology of the body and the pharmacology of what aspirin does should understand that the blockade of the production of important prostaglandins is more harmful than beneficial. Simply stating that aspirin thins the blood and reduces platelet aggregation is being irresponsible to the patient and shows the lack of understanding on the doctor's part. Read "What Causes Heart Attacks" in the articles list for more information on why this is the wrong mindset.
MILLIONS OF AMERICANS are being urged to take an-aspirin-a-day to prevent a stroke and heart attack. But a major research study in Canada found this actually increased the risk of stroke and heart attack in 40% of the people who took it! Three other studies from Germany, Britain, and here in the U.S. support the finding.
But that's not the worst of it. New research shows that such long-term aspirin use can make you blind by increasing your risk of macular degeneration, and even increasing your risk of cataracts by up to 44 percent! Those are bad odds. Macular degeneration is already the leading cause of blindness in people over 55 in our country, and doctors still have no effective treatments. If this current aspirin-a-day craze continues, we could be looking at a wave of blindness in the years to come.
The drug companies that make and market aspirin have a huge vested interest in convincing people that "an aspirin a day keeps the heart attack away." The basis for this belief is that aspirin decreases the risk of heart attack by decreasing the “stickiness” of platelets (the substance that helps in clotting blood), and in turn, decreases thrombus formation.
Depending on who has done the study on this subject, who are you to believe? Of course, aspirin makers will make the claim that it prevents heart attacks. But what do independent, non-biased studies say? Many studies have come along to prove otherwise.
According to British researchers at the Wolfson Institute of Preventive Medicine in London, the daily aspirin regimen might actually do more harm than good. Researchers identified more than 5,000 male subjects, between 45 and 69 years old, who were at increased risk of coronary heart disease, but had not previously had heart trouble. The men had been randomly divided into four different treatment groups to accurately establish the effect of aspirin. The men with higher blood pressure not only weren't protected by the aspirin, but they risked possible serious bleeding (intestinal bleeding included). Even in men with low blood pressure, the benefit did not necessarily outweigh the risk of bleeding.
In 1988, another research study found that some high risk men who took daily aspirin had fewer heart attacks, but had more strokes. Even these researchers never recommended the once-a-day aspirin regimen. Some studies like this are used to mislead the public. They do this by stating only half of the results, such as informing those that aspirin did prevent heart attacks, but they did not disclose the finding that aspirin increased the risk of stroke.
However, the pharmaceutical industry immediately began a massive press release campaign which distorted the research report. The press releases gave the impression that the daily aspirin was a sure-fire way to prevent heart attacks. The news was picked up by most newspapers and even medical doctors began "prescribing" aspirin as a preventative measure. Once the seeds of deception are planted, these are hard to uproot.
Thanks in part to this deceptive marketing campaign, Americans now take more than 25 million aspirin tablets every day, despite the facts that:
1. 1,600 children die each year from allergic reactions to aspirin.
2. Patients with blockage of arteries to the brain are three times more likely to have a stroke if they are taking aspirin.
3. Dyspepsia and gastrointestinal hemorrhage occur in 31% of those taking 300 mgs of aspirin per day.
4. You can also lose up to a teaspoon of blood per day, through the rectum, by taking daily doses of aspirin.
5. Low doses of aspirin (one baby aspirin) can increase the risk of brain hemorrhage.
6. Other side effects of daily aspirin usage can include anemia, bleeding ulcers, confusion and dizziness and numerous other problems.
Don’t believe me? Look it up.
SOURCES:
1. "Determination of who may derive most benefit from aspirin in primary prevention: subgroup results from a randomised controlled trial," British Medical Journal, July 1, 2000.
2. "FDA warns aspirin makers." Science News, March 12, 1988 v133 n11 p165(1).
3. "The preliminary report of the findings of the aspirin component of the ongoing Physicians' Health Study; the FDA perspective on aspirin for the primary prevention of myocardial infarction." Journal of the American Medical Association (JAMA) June 3, 1988 v259 n21 p3158(3).
4. "Don't jump the gun with aspirin; there are surer ways to help prevent (heart attacks), ones that don't increase stroke risk," Medical World News, May 23, 1988 v29 n10 p50(1).
5. "High-risk pain pills: though their use is regulated, many common pain remedies can be dangerous, particularly if combined with alcohol or other drugs," The Atlantic, Dec. 1989 v264 n6 p36(5).
When large health and environmental groups, which affect public policy, are being funded by industries with agendas, it is possible that scientists who claim to be objective may ignore important health, safety, and environmental considerations.
Bayer donates over $500,000 a year to the American Heart Association (AHA), which may explain why the AHA has endorsed only Bayer aspirin. Bayer also contributes over $500,000 a year to the American Diabetes Association, is a sustaining member of the American Medical Writer's Association, and contributes to the American Veterinary Medicine Association, the Arthritis Foundation, the Biotechnology Institute, and the Environmental Sensitivities Research Institute. Bayer also supports the Heartland Institute, an "independent research policy group". Bayer is a member organization of the National Center for Food and Agricultural Policy, which is supposed to maintain publicly available national databases on pesticide use, develop methods and data systems to improve the estimation of pesticide benefits and prepare reports, articles, and testimony on pesticide policy issues.
Bayer donates money to the Alliance for the Prudent Use of Antibiotics, a scientific front group that also receives donations from Bristol-Myers Squibb, Johnson & Johnson, Procter & Gamble Pharmaceutical and SmithKline Beecham Pharmaceuticals Inc., which may explain their watered-down web page which claims that antibiotic resistant bacteria is a natural phenomenon and that "Although the scientific evidence does indicate that antibiotic use in animals is a key factor promoting resistance, the validity and reliability of the data have been questioned."
In addition, Bayer donates exorbitant amounts of money to political parties, especially in the United States. In fact, between 1 January 1999 and 30 June 2000 alone, Bayer donated $134,511 to the Republican party and $40,150 to the Democrats, for a grand total of $174,661.
Bayer also admitted to supporting the "further education" of doctors in Portugal by paying for trips around the world in an attempt to influence prescription writing. According to former pharmaceuticals salesman Alfredo Pequito, Bayer invested approximately DM 100,000 in the first 5 months of 1995 to promote the prescribing of Ciproxin in Portugal. He reports that amounts of up to DM 5,000 were deposited in travel agencies for various doctors. The money was not always used for conventions, but for other uses such as family trips or even exchanged for cash. The head of the Portuguese State Medical Board Carlos Ribeira believes this brings the ethical and moral ideals of the medical profession in question. He has announced that he intends to take legal action. The public prosecutors and the Ministry of Health have also begun investigations.
What does all this mean? It means that money influences decision making and approval setting. When a company, like Bayer, invests huge sums of money to a cause, that agent of cause will find it very difficult to go against the wishes of their donors. In effect, companies like Bayer are trying to influence decision making financially.
According to a study in the January 7, 2004 issue of the "Journal of the National Cancer Institute", regular aspirin use for 20 years or more may be associated with an increased risk of pancreatic cancer in women, the fourth leading cause of cancer-related deaths in the United States.
Eva S. Schernhammer, M.D., Dr.P.H., of the Brigham and Women's Hospital and Harvard Medical School in Boston, and her colleagues examined the association between aspirin use and risk of pancreatic cancer among 88,378 women participating in the Nurses' Health Study. The information used in the study was based on questions about aspirin use asked on biennial questionnaires beginning in 1980. Among those women, 34% were current regular aspirin users, defined as women who took two or more 325 mg aspirin tablets per week. The remaining women were non-regular aspirin users who took less than 2 tablets per week.
When the investigators compared women who had reported consistent, regular aspirin use with women who were non-users during the same time period, they found that the risk of pancreatic cancer increased with increasing aspirin dose. Compared with nonusers, women who took 14 or more aspirin tablets per week had an 86% increased risk of pancreatic cancer.
In an accompanying editorial, John A. Baron, M.D., of Dartmouth Medical School, writes, "There are no easy answers to the question of what aspirin and other NSAIDs do to pancreatic carcinogenesis. The findings by Schernhammer et al. are provocative and force us to think carefully about the actions of aspirin and other NSAIDs and the mechanisms underlying pancreatic cancer. Fortunately, conflicting data from diverse threads of research are often a very effective push toward scientific progress."
According to a study done in England in the December 5, 2013 issue of the "PLOS-one", when aspirin is used for primary prevention of CVD the absolute harms exceed the benefits.
The study found that use of aspirin for primary prevention of CVD is associated with net harm due to increased potential for bleeding.
Risks were increased by 37% for gastrointestinal bleeds, 54%-66% for major bleeds, and 32%-38% for haemorrhagic stroke.
The full study can be seen at this link.
According to a study in the February 25, 2013 issue of "JAMA Internal Medicine", regular aspirin use is associated with increased risk of incident neovascular AMD, independent of a history of cardiovascular disease and smoking.
The study showed that persons who were regular aspirin users were more likely to have incident neovascular AMD (Age-Related Macular Degeneration).
The study showed that persons who were regular aspirin users had a 146% increased risk of developing neovascular AMD
The study can be viewed here.
Reuters Health reported that selective and nonselective nonsteroidal anti-inflammatory drugs (NSAIDs) are associated with an increased risk of a first MI (Myocardial Infarction/Heart Attack), results of a British Medical Journal observational study suggest (BMJ 2005;330).
Diclofenac and ibuprofen seem to pose about as much risk as the COX-2 inhibitor rofecoxib, the study authors say. Rofecoxib (Vioxx) was withdrawn from the pharmaceutical market at the end of September 2004 after use of the drug was tied to adverse cardiac effects. Since then, however, questions remain, such as whether all NSAIDs share these harmful effects.
Drs. Julia Hippisley-Cox and Carol Coupland, from the University of Nottingham, UK, conducted a population-based nested case-control study using the QRESEARCH database of information from UK general practices. They report their findings in the June 11th issue of the British Medical Journal. Their study included 9218 cases of a first MI in people between the ages of 25 and 100 during study period from 2000 to 2004, and 86,349 controls matched by age, calendar time, gender and practice.
"Given the high prevalence of the use of these drugs in elderly people and the increased risk of myocardial infarction with age, even the relatively large number of patients needed to harm could have considerable implications for public health," they note. "We think that enough concerns exist to warrant a reconsideration of the cardiovascular safety of all NSAIDs," the investigators conclude.
Although aspirin and acetaminophen work in slightly different ways, it is important to include some information about the dangers of acetaminophen. Acetaminophen (Tylenol) causes more than half the acute liver failure in the United States. A 6-year multicenter study showed that acute liver failure cases attributable to acetaminophen increased from 28% in 1998 to 51% in 2003 (Larson AM, Hepatology 2005;42:1364-1372).
According to the FDA, acetaminophen toxicity annually causes 56,600 ER visits, 26,000 hospitalizations, and 458 deaths in the United States. Adults should not take more than 4 grams daily (that is equal to 8 extra strength tablets). If you have impaired liver function or drink alcohol regularly, you should not take more than 2 grams daily (that is 4 extra strength tablets). Anyone who drinks more than three alcoholic drinks a day should avoid acetaminophen entirely.
What does platelet stickiness have to do with preventing heart attacks?
The subject of heart attacks and coronary artery disease is too vast to be completely covered in this article. The focus, then, will be the basic scenarios of heart attacks and how the belief came to be that aspirin could help prevent them.
There are three basic scenarios about how heart attacks can occur. One, which is the most common, is due to a partial or complete blockage of a coronary artery (arteries that supply the heart with oxygen and nutrients). This most often occurs due to a blood clot. Another scenario is that arrhythmias can prevent the heart from pumping enough blood to ensure its own supply of oxygen and nutrients. The last basic scenario is due to a rupture of a coronary blood vessel (aneurysm) which can cause internal bleeding and disrupt the heart’s blood flow.
The belief that a daily aspirin regimen can prevent heart attacks ties in with the first scenario, partial or complete blockage of a coronary artery. Typically, coronary arteries can be narrowed by years of a disease process which causes narrowing of the lumen (the space inside the artery where blood flows) by plaque build up, a process called atherosclerosis. This plaque can be composed of cholesterol deposits, proteins, calcium, and excess smooth muscle cells. In this scenario, the artery walls thicken over time, decreasing the available blood that nourishes the heart muscle. Once the lumen become narrowed, it can be blocked by many situations, such as a spasm of the artery or a blood clot that has traveled from a distant site and has become lodged in the narrow lumen. When one of these narrowed arteries becomes completely blocked, the result is a heart attack.
Remember that the subject of heart attacks is extremely vast and we are trying to stay with the basic ideas of them, but it is important to understand a few processes that lead to this blockage situation. How does this arterial disease come about? There are many misconceptions and misunderstanding when it comes to atherosclerosis. The following will be a basic explanation, grossly over simplified, but will give the reader a common sense understanding.
Firstly, there is no such thing as “good” cholesterol or “bad” cholesterol. The medical field labels HDL as “good” and LDL as “bad”. This is completely wrong. Each of these two forms of cholesterol serves a purpose in the body. HDL and LDL each have a role to play, and it is their roles that make each one essential. The only time that one can call cholesterol “bad” is when it is in an unnatural form or when it has been oxidized (this require a lengthy explanation, but it beyond the scope of this article).
HDL takes cholesterol from different areas of the body and brings it to the liver so that the liver may use it for constructing hormones (cortisol, estrogens, testosterone, aldosterone, etc.), producing bile acids, repairing membranes, making vitamin D, and so on. LDL takes cholesterol from the liver and transports it to tissues throughout the body. The cholesterol transported by LDLs is then used, by cells, for cell membrane repair, making hormones, etc.
Given this information, how did LDL become to be known as “bad” cholesterol? It is when LDL becomes oxidized that it poses problems. If it is not oxidized, it is simply functioning as it should. Let’s focus on LDL’s and relate it to atherosclerosis. When the lining of an artery becomes damaged, it must be repaired. How is it repaired? By LDL (and other constituents) coming in and attempting to repair the leak or damaged area. The cholesterol that LDL brings to the site will be used to manufacture new cell membranes, and so on. In this process of repair, platelets attach to the leaky vessel in order to stop blood from flowing out of the system. This process of plugging a leak and then repairing the cells of the vessel are what is supposed to happen, or we would die. Sometimes the repair process can malfunction and build layer upon layer, causing the arterial lumen to narrow too much. If the LDL becomes oxidized, it will essentially become brittle. If brittle, it will need to be repaired again and again. Platelets come in to plug the leak, LDL comes in for membrane repair, and so on in an endless cycle.
The key is to understand why the process is not repairing correctly. The mistake is to try to stop a necessary function by focusing on the wrong physiology. Ask yourself, why do vessel get damaged? Two examples could be dehydration and/or lack of certain key nutrients. Blood is part fluid and part cells. One can imagine that if you reduce the fluid level flowing through a vessel, the contents would become very abrasive to the inside lining of that vessel, causing greater wear and tear than the vessel could handle. In essence, requiring constant repair from these shearing forces. On the other hand, lack of vitamin C will inhibit collagen synthesis, which will lead to faulty repair of flexible vessels and will lead to “brittle” vessels. These brittle vessels will then need constant repair as well. So, given the two scenarios of dehydration and lack of vitamin C, one could rehydrate the body and supply it with the proper nutrients, preventing the need for excessive repair, preventing the build up of repair products, preventing narrowing of the lumen, preventing a source of heart attacks. This is over simplified, but the idea is made clear.
Now take the aspirin scenario. If you take aspirin to prevent platelet stickiness, to prevent a heart attack, you are creating a monster. You don’t need to be a doctor to understand why, given the above example. By inhibiting the clotting process, you are inhibiting the body’s ability to plug a leaky vessel. Of all the things that can go wrong with taking aspirin on a daily basis, this reason is one that will cause great harm to the body. The inhibition of platelet stickiness does not only affect the vessels of the heart, it affects every vessel in the body. Think of what the body must do for repairs when one of its key defenses is shut down. It is a disaster waiting to happen.
As stated many times, this is a very simplified example. Taking daily doses of aspirin will prevent platelets from sticking and clumping together, but in the long run, is this a function of the body that you really want to inhibit? In theory, you could actually bleed to death internally if you stop the necessary clotting process. Taking daily doses of aspirin is a decision that needs to be examined closely. Better choices need to be observed. Better understanding of the physiology of the body need to be observed.
Hopefully this will help the reader to begin to understand the flawed thinking behind a daily aspirin regimen. A concerned patient should always question treatments. A concerned patient should ask questions until they completely understand how they are being treated. A concerned patient should always know the risks and benefits of every mode of treatment prescribed to them. Never blindly follow a treatment.
By the way, did you know that vitamin E will basically do the same thing as aspirin, except it won’t shut down the clotting process, and it won’t have harmful side effects. It will, if effect, make platelets more slippery. Vitamin E is an antioxidant and will prevent the oxidation of LDLs (as discussed above). Vitamin E is more protective than aspirin in the prevention of heart attacks. CAUTION: Beware of studies that say the opposite. Some studies claim that there is no benefit, or that there is actually harm caused by taking vitamin E. These studies did not use the natural form, they used the synthetic form which is called DL-alpha-tocopherol. The natural form that provides the benefits is D-alpha-tocopherol (minus the “L”).
Gamma-Linolenic Acid (GLA)- is the active ingredient in borage oil, black currant seed oil, flaxseed oil, and primrose oil. It is an omega-6 fatty acid. It suppresses the production of certain prostaglandins similar to the way that aspirin does. It is a safer, natural substance.
Beta Carotene - Beta carotene has mild blood clotting retarding effects. Several studies show an inverse relationship of the consumption of fruits and vegetables high in beta carotene and subsequent death from coronary artery disease. Carrots and carrot juice are also alkaline forming foods. Always use caution with Beta carotene and vitamin A when pregnant.
Bioflavonoids - Bioflavonoids can lower LDL-cholesterol levels and inhibit platelet stickiness much like what aspirin is used for. They are special antioxidant compounds found in many fruits, especially berries and citrus. Sources of bioflavonoids include: peppers, buckwheat, black currants, apricots, blackberries, cherries, grapefruit, grapes, lemons, oranges, plums, prunes, and rose hips. Some better known bioflavonoids include catechin, hesperidin, rutin, quercetin, pycnogenol, pronogenol, and polyphenols.
Vitamin B6- prevents accumulation of high levels of the amino acid homocysteine implicated as one of the tissue injuring substances initiating atherosclerosis. Vitamin B6 has blood clot retarding effects. Vitamin B6 deficiency has been associated with a greater risk of coronary artery disease, elevated serum cholesterol and atherosclerosis.
Vitamin E - is otherwise known as alpha-tocopherol. High doses have been shown to retard blood clotting. Caution should be exercised if one is using both aspirin and vitamin E because the combination has a synergistic effect. Studies indicate that supplementation of as little as 200 I.U. daily in men can reduce the risk of a heart attack by 46%; in women the risk reduction is by 26%. The natural forms of vitamin E are d-alpha-tocopherol, d-alpha-tocopheryl acetate, d-alpha-tocopheryl succinate and mixed tocopherols. The synthetic forms are dl-alpha-tocopherol, dl-alpha-tocopheryl acetate or dl-alpha-tocopheryl succinate. All the synthetic forms contain an "L" after the "D". NEVER use these "L" containing synthetic vitamin E's.
Garlic - is probably the best known herb that lowers cholesterol (by up to 10%) and triglycerides (by up to 13%) while raising HDL-cholesterol (by up to 31%), prevents thrombus formation and lowers blood pressure. It prevents platelet stickiness and has natural anti-bacterial, anti-fungal and anti-parasitic properties.
Magnesium - has anticoagulant properties which, when combined with vitamin E can produce significant blood clotting reduction. Doctors frequently prescribe calcium channel blockers to treat heart problems. Magnesium has been referred to as nature's calcium channel blocker. The problem is that, in order to correct an arrhythmia or eliminate angina, it usually has to be given at dosages far above those that can safely be tolerated in oral supplement form. The only way to get around this problem is through the intravenous or intramuscular injection route. Many people can learn to give themselves intramuscular injections of magnesium and help reverse many cardiovascular problems naturally. In practice it is always wise to balance magnesium intake with both calcium and potassium.
Omega-3-Fatty Acids (EPA oils) -reduces cholesterol and prevents platelet stickiness. Good dietary sources include flax seed oil, rice bran oil, trout, mackerel, salmon, herring, sardines, cod, halibut and shark.
Onions - have effects on lowering blood pressure and cholesterol as well as retarding platelet stickiness in much the same way as garlic.
White willow bark (Salix alba) - contains salicin from which aspirin is manufactured. While not as potent as aspirin, white willow has very similar properties without the gastrointestinal side effects at therapeutic dosages. Overdoses can, however, produce toxicity similar to that seen with aspirin overdoses.
Possible reactions to acetaminophen include three serious skin diseases whose symptoms can include rash, blisters and, in the worst case, widespread damage to the surface of skin. If you are taking acetaminophen and develop a rash or other skin reaction, stop taking the product immediately and seek medical attention right away.
Acetaminophen is the generic name of a common active ingredient included in numerous prescription and non-prescription medicines. Tylenol is one brand name of the pain reliever sold over the counter, but acetaminophen is also available as a generic under various names. It is also used in combination with other medicines, including opioids for pain and medicines to treat colds, coughs, allergy, headaches and trouble sleeping.
It is extremely important that people recognize and react quickly to the initial symptoms of these rare but serious, side effects, which are potentially fatal.
Other drugs used to treat fever and pain, such as nonsteroidal anti-inflammatory drugs including ibuprofen and naproxen, already carry warnings about the risk of serious skin reactions. Advil and Motrin are among the common brand names that include ibuprofen as an active ingredient. Aleve and Midol Extended Relief are among the best-known brand names that include naproxen as an active ingredient.
Stevens-Johnson Syndrome (SJS) and toxic epidermal necrolysis (TEN) are the two most serious skin reactions linked in rare cases to acetaminophen. They usually require hospitalization and can cause death. Problems usually begin with flu-like symptoms followed by rash, blistering and extensive damage to the surfaces of the skin. Recovery can take weeks or months, and possible complications include scarring, changes in skin pigmentation, blindness and damage to internal organs. A third skin reaction, acute generalized exanthematous pustulosis (AGEP), usually resolves within two weeks of stopping the medication that caused the problem. A serious skin reaction can occur at any time, even if you've taken acetaminophen previously without a problem. There is currently no way of predicting who might be at higher risk. If you've ever had a skin reaction when taking acetaminophen, don't take the drug again and discuss alternate pain relievers/fever reducers with your health care professional.
Prior to deciding to add a warning about skin reactions to products containing acetaminophen, FDA reviewed medical literature and its own database, the FDA Adverse Event Reporting System (FAERS). A search of FAERS uncovered 107 cases from 1969 to 2012, resulting in 67 hospitalizations and 12 deaths. Most cases involved single-ingredient acetaminophen products; the cases were categorized as either probable or possible cases associated with acetaminophen. A small number of cases, just over two dozen, are documented in medical literature, with cases involving people of various ages.
The FDA says that the agency continues to consider the benefits of this medication to outweigh the risks.
My note to readers: Acetaminophen injury is the leading cause for calls to Poison Control Centers (>100,000/year) and accounts for more than 56,000 emergency room visits, 2,600 hospitalizations, and an estimated 458 deaths due to acute liver failure each year. Data from the U.S. Acute Liver Failure Study Group registry of more than 700 patients with acute liver failure across the United States implicates acetaminophen poisoning in nearly 50% of all acute liver failure in this country. Available in many single or combination products, acetaminophen produces more than 1 billion US dollars in annual sales for Tylenol products alone.
There you have it! The FDA continues to say that the benefits outweigh the risks. Yes, if you mean the financial benefits. Always the might dollar over the health of the population.
Let's have a discussion about the article in the link above.
The aforementioned article states, “New US research has found a link between taking a daily aspirin and a higher risk of melanoma in men, the most dangerous form of skin cancer. Carried out by researchers at Northwestern University, the study looked at medical records from 195,140 patients aged 18-89, who had no prior history of melanoma. From this base, 1,187 of the patients were aspirin exposed, with the researchers only including patients who had been taking aspirin daily for at least one year at a dose of 81 or 325 mg. All patients were followed for at least five years to see if melanoma occurred over time. The team found that from the 1,187 aspirin-exposed patients, 2.19 percent had a subsequent diagnosis for melanoma, compared to 0.86 percent of those in aspirin-unexposed patients. However, when the researchers looked at the groups by gender, they found that men exposed to aspirin had nearly double the risk of melanoma than the men who were unexposed.”
The study's senior author, Dr. Beatrice Nardone, goes on for the remainder of the article to interject her opinion about the information.
Let's dissect the information given so far. We are told that out of 195,140 patients, whose ages ranged from 18-89, the authors of the study chose 1,187 patients that were “exposed” to aspirin and only took patients who self reported a daily dose of 81mg-325mg per day. The article also states that 2.19% were diagnosed with melanoma compared to 0.86% diagnosed that did not report using aspirin.
At this point, my instincts are to look at the actual study to help clarify what is going on. I see a lot of room for bias and error.
The actual study used to write this article is listed as: DOI: 10.1016/j.jaad.2018.03.031 at the Journal of the American Academy of Dermatology website. At the time of my listing of this information, the “Accepted Manuscript” of this study was provided. In this manuscript, there was no abstract, no methods/procedures, or any other detailed information about the study provides (other than 2 data tables).
From here on out, I will be referring to “the study” and “the article” to clarify information.
Right from the start, there is a wording difference between the article and the study. The article uses the word “melanoma” and the study uses they term “malignant melanoma.” There is a HUGE difference between the two terms. There are benign/non-malignant forms of melanoma and there are malignant forms of melanoma. It is extremely important to make this distinction. This is a gross misrepresentation by the author of the article and the doctor who is stating her opinion throughout the article to not make this clarification.
The stated purpose of the study “was to determine if there was or was not a detectable risk for malignant melanoma (MM) after 1 year or more of chronic aspirin exposure.”
Now let's match the study information with the article information.
The study authors said they used a medical record data repository (with greater than 5 million patients) to search adverse drug events from January 2005- December 2006. “The study inclusion criteria consisted of all patients, aged 18-89 years, no prior history of MM and a minimum follow-up time of 5 years after continuous once-daily aspirin exposure for 1 year or more. The control population consisted of all patients within the same time frame, but with no documentation of aspirin exposure.”
Bored yet? Clear as mud?
The study has a different way of displaying the number of patients and subsequent categories.
From the total number of patients researched (195,140): a) 1,187 self reported to be “aspirin exposed.” Of that number 26 were diagnosed with malignant melanoma (2.19%). b) 193,953 self reported to be “aspirin un-exposed.” Of that number 1,676 were diagnosed with malignant melanoma (0.86%).
The study goes on to state that the “Relative risk (RR) for malignant melanoma after aspirin exposure was determined by logistic regression analysis with a 95% Confidence Interval (CI).
In a nutshell, what a 95% CI implies is that if you did an experiment over and over, many many times, that there would be a 95% chance that you would come out with the same results. So, a 95% CI is very high and likely. A small problem here is that there was no experiment done. It was only selective research from a database. Since the criteria for selection was self reported, there is room for error.
Finally, the study uses diagnostic codes to refer to the form of malignant melanoma detected. The codes are ICD-9: 172.0-172.9 (malignant melanoma of the skin of the lip) and ICD-10: C43.0-C43.9 (malignant melanoma of the lip).
With that said, the study did prove that there was a “detectable risk”. How accurate it truly is, you can NEVER know.
In my opinion, as you may have noticed from my postings on aspirin, there are many many harms that come from aspirin use. A 2% chance of getting malignant melanoma may seem insignificant to some, but it still adds to the proof that aspirin use is not an overall beneficial toxin on which to rely.